Temperature monitoring breaks at exactly the moments when clinical teams need visibility most: patient transport, equipment handoffs, and care transitions.
Perioperative departments rely on esophageal probes during surgery and face monitoring gaps the instant patients move to recovery, enter the MRI suite, or transition to ambulatory discharge. Those gaps create documentation challenges, workflow friction, and operational risk. Power-free temperature indicators stay with the patient across every handoff without adding equipment complexity, maintenance burden, or workflow steps.
The monitoring continuity question in perioperative workflows
Clinical guidelines require continuous temperature monitoring during anesthesia to prevent hypothermia and detect hyperthermia. Facilities invest in esophageal probes, electronic sensors, and monitoring systems that deliver precision core temperature readings throughout surgery.
Then patients move. Electronic monitors disconnect during transport. Equipment changeover delays readings when PACU nurses manage multiple recovering patients simultaneously. MRI procedures require the complete removal of electronic devices. Esophageal probes deliver precision but demand invasive placement and continuous electronic connection that ends the moment the OR handoff begins.
The question is how to maintain temperature awareness across care transitions without adding workflow complexity, equipment handoffs, or documentation gaps.
How power-free temperature indicators change operational control
FeverScan is applied to the forehead and displays temperature directionally without batteries, calibration, or electronic connection. It stays with the patient during transport, MRI procedures, and PACU handoffs when traditional monitoring is disconnected or impractical.
One visual indicator works across OR, transport, and recovery instead of multiple monitoring handoffs. The cost structure shifts from capital equipment and maintenance contracts to disposable supplies that facilities control based on clinical protocols. Clinical teams decide when and where to apply passive monitoring without biomedical engineering involvement or equipment integration.
Procurement and clinical teams control application timing. Apply at anesthesia start, and the indicator travels with the patient through discharge while electronic monitors remain with the OR. Temperature awareness continues without modifying existing handoff protocols.
FeverScan’s functional role in temperature monitoring
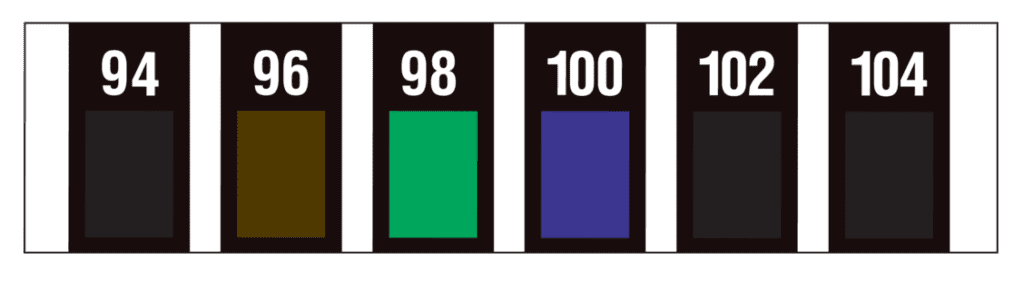
FeverScan uses thermochromic liquid crystal technology, which responds to body heat through skin contact. The indicator displays core-adjusted temperature trends and directional changes. It serves as a redundant monitoring layer and visual screening tool during workflow transitions.
Staff verify temperature status at a glance without reconnecting electronic equipment. The indicator works as operational support.
Common misconception: Some teams assume passive indicators substitute for electronic monitoring during anesthesia. FeverScan complements guideline-required devices by filling visibility gaps during transitions where electronic monitoring is disconnected, impractical, or unavailable. Clinical protocols determine which monitoring method fits each scenario.
Second misconception: Teams may expect directional indicators to deliver the same precision as esophageal probes. FeverScan provides temperature trend awareness, not core measurement. The operational value appears in workflow continuity, not in replacing validated monitoring devices.
Which clinical environments see operational benefits
Surgery centers managing ambulatory anesthesia cases with rapid patient turnover benefit from indicators that move with patients across OR, transport, and recovery phases. PACU departments handling multiple post-operative patients during initial triage gain visual screening tools that work without equipment reconnection.
Facilities conducting MRI procedures use indicators where electronic monitors must be removed. Pediatric departments apply non-invasive temperature monitoring for conscious patients who may not tolerate esophageal placement.
Disaster response and mass casualty scenarios face limited monitoring infrastructure. Power-free indicators function without electrical supply, calibration, or technical support.
Consider an outpatient surgery center managing daily cases across OR, transport, recovery, and discharge with minimal biomedical equipment. Indicators applied at case start provide temperature awareness through every transition without adding equipment handoffs, calibration protocols, or maintenance schedules. Clinical staff document readings using the same process as electronic monitors.
How FeverScan fits into existing perioperative protocols
Apply the indicator to the forehead at anesthesia start or during PACU admission. Clinical staff read the visual display and document in the patient record using the same process as electronic monitors. The indicator remains visible during transport and MRI without removal.
No integration with electronic systems, biomedical calibration, or multi-use sterilization protocols required. Temperature monitoring supports clinical guidelines without changing fundamental handoff workflows. Staff verify status visually during existing documentation touchpoints.
Comparison to invasive and electronic monitoring methods
Esophageal probes deliver precision core temperature but require invasive placement and continuous electronic connection. Electronic forehead sensors provide accurate readings but need power, calibration, and capital equipment investment.
FeverScan provides directional temperature trends without invasive placement, power requirements, or maintenance. Clinical guidance determines which monitoring method fits each scenario. FeverScan complements validated devices.
The operational fit appears in workflow gaps, resource-limited settings, redundancy layers, and non-invasive monitoring scenarios where electronic infrastructure is disconnected or unavailable.
Counterargument worth addressing: Some procurement teams question whether disposable indicators cost more over time than reusable electronic sensors. Total cost of ownership includes capital equipment investment, maintenance contracts, calibration protocols, sterilization processes, and biomedical engineering support. Disposable indicators eliminate those ongoing costs. Facilities compare equipment and maintenance burden against disposable unit cost per procedure based on case volume and monitoring requirements.

Cost and infection control considerations
Disposable format eliminates multi-use sterilization protocols and cross-contamination risk between patients. No capital equipment investment or maintenance contracts required. Single-use design simplifies procurement and inventory management compared to tracking, cleaning, and calibrating reusable devices.
MRI-safe and latex-free construction reduces contraindication protocols. Procurement teams evaluate the total cost of ownership: equipment plus maintenance plus sterilization versus the disposable unit cost per procedure.
Integration planning for procurement and clinical teams
Technical evaluators assess workflow integration points: OR handoffs, transport, PACU admission, MRI procedures, and discharge. Procurement teams evaluate cost structure and inventory management compared to electronic monitoring alternatives.
Clinical staff pilot indicators in target use cases such as ambulatory surgery, pediatric recovery, and MRI transport. Biomedical engineering reviews the elimination of calibration and maintenance requirements. Quality and infection control teams validate disposable protocols and documentation procedures.
Integration starts with identifying specific workflow gaps where electronic monitoring disconnects or becomes impractical. Facilities define clinical scenarios where directional temperature trends deliver operational value.
Conclusion
Temperature monitoring gaps during perioperative transitions represent an operational risk that facilities can address. Power-free indicators provide continuous visual awareness without adding equipment complexity, workflow steps, or maintenance burden. Facilities gain monitoring flexibility that adapts to ambulatory surgery, PACU handoffs, MRI procedures, pediatric cases, and resource-limited settings where traditional electronic monitoring is impractical.
Next step: Review how FeverScan fits your facility’s anesthesia and PACU monitoring protocols, procurement priorities, and workflow transition points by visiting the FeverScan product page.
—
You might also like :







